Fill Your Tb Test Form
Different PDF Templates
Form 6059B Customs Declaration - Compliance with the CBP 6059B helps keep traveling straightforward.
For those seeking guidance on workplace policies, the Missouri Employee Handbook is an indispensable resource that encapsulates key procedures and expectations for employees. To facilitate your understanding, you can access the form by clicking here for the Employee Handbook download.
Mechanics Lien California - A valid Mechanics Lien must include specific details about the work performed.
Similar forms
The Immunization Record form serves a similar purpose to the TB Test form by documenting a patient's vaccination history. This record includes details such as the type of vaccine administered, the date it was given, and the healthcare provider's signature. Like the TB Test form, it requires completion of all sections to be considered valid. Both documents are essential for ensuring that individuals are protected against infectious diseases and for meeting school or employment requirements.
Understanding the importance of proper documentation in healthcare, the EDD DE 2501 form is one such crucial form aimed at assisting individuals in California with their disability claims. It enables patients to disclose pertinent information about their medical backgrounds while ensuring they receive the necessary financial support during their period of need. If you require help with the paperwork, you can easily Fill PDF Forms to streamline the process and avoid any potential setbacks.
The Health Screening Questionnaire is another document that resembles the TB Test form. It collects information about a patient’s health status, including any symptoms or exposures to communicable diseases. This questionnaire may be used in various settings, such as schools or workplaces, to assess the risk of disease transmission. Both documents emphasize the importance of thorough completion to ensure accurate health assessments.
The Laboratory Test Results form is similar in that it provides essential health information based on tests conducted. This form includes details such as the type of test, results, and the date of testing. Just like the TB Test form, it must be filled out completely to be valid. Both documents play a crucial role in monitoring and managing health conditions effectively.
The Medical History Form also shares similarities with the TB Test form. It gathers comprehensive information about a patient's past medical conditions, surgeries, and family health history. Both documents require detailed information to ensure that healthcare providers can make informed decisions about a patient’s care. The completeness of these forms is vital for accurate medical assessments.
The Consent for Treatment form is another document that parallels the TB Test form. It ensures that patients understand and agree to the procedures being performed, including testing like the TB skin test. Both forms require signatures from healthcare providers and patients, underscoring the importance of informed consent in medical care.
The Patient Registration Form is similar in that it collects essential demographic and contact information from patients. This form often includes sections for health insurance details and emergency contacts. Like the TB Test form, it must be completed in full to facilitate effective communication and care coordination between the patient and healthcare providers.
The Release of Medical Information form also shares characteristics with the TB Test form. It allows patients to authorize the sharing of their health information with other parties, such as specialists or employers. Both documents require careful completion to ensure that patient privacy is maintained while allowing for necessary information exchange.
The Referral Form is another document that resembles the TB Test form. It is used when a healthcare provider recommends a patient to see a specialist. This form includes details about the patient’s condition and the reason for the referral. Similar to the TB Test form, it must be filled out completely to ensure that the receiving provider has all necessary information for effective care.
The Follow-Up Care Plan is akin to the TB Test form in that it outlines the next steps in a patient’s treatment after an initial assessment. This document may include recommendations for further testing or lifestyle changes. Both forms emphasize the importance of thorough documentation to ensure continuity of care and effective patient management.
Finally, the Allergy Information Form is similar to the TB Test form as it collects critical data about a patient’s allergies and sensitivities. This information is vital for healthcare providers to avoid potential allergic reactions during treatment. Both documents require complete and accurate information to ensure patient safety and effective healthcare delivery.
Instructions on Writing Tb Test
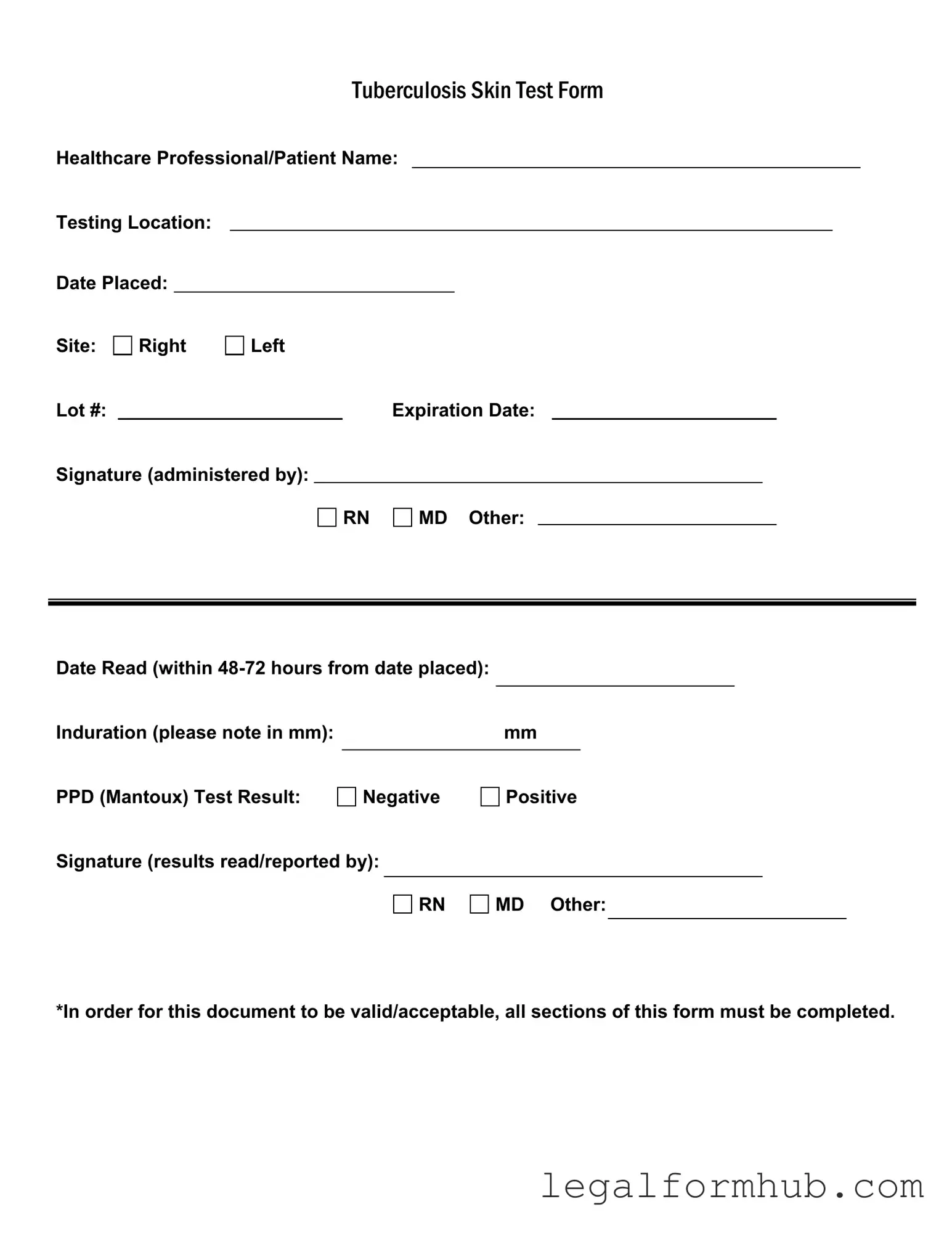
Completing the TB Test form accurately is essential for ensuring proper documentation and follow-up care. After filling out the form, it will be submitted to the appropriate healthcare provider or institution for record-keeping and further action. Below are the steps to guide you through the process of filling out the form.
- Start by entering the Healthcare Professional/Patient Name at the top of the form.
- Next, fill in the Testing Location where the test is being administered.
- Record the Date Placed—this is the date when the test is conducted.
- Indicate the Site of the test by marking either Right or Left.
- Enter the Lot # of the test material used.
- Fill in the Expiration Date of the test material.
- Provide the Signature of the healthcare professional administering the test, selecting from RN, MD, or Other.
- Record the Date Read—this must be within 48-72 hours from the date placed.
- Measure and note the Induration in millimeters (mm).
- Indicate the PPD (Mantoux) Test Result by marking either Negative or Positive.
- Finally, provide the Signature of the healthcare professional who read or reported the results, selecting from RN, MD, or Other.
Misconceptions
Understanding the Tuberculosis (TB) Test form can be challenging due to various misconceptions. Here are ten common misunderstandings about the TB Test form and clarifications for each.
-
All sections of the form are optional.
In reality, every section of the TB Test form must be completed for it to be valid and acceptable. Incomplete forms may lead to delays in processing results.
-
The test can be read anytime after placement.
The test must be read within 48 to 72 hours after placement. Reading the test outside this window can result in inaccurate interpretations.
-
A negative result means no exposure to TB.
A negative result indicates that no active TB infection was detected at the time of testing. However, it does not rule out past exposure or latent TB infection.
-
Only healthcare professionals can administer the test.
While it is typically administered by trained healthcare professionals, individuals with proper training may also be authorized to perform the test.
-
The induration measurement is not important.
The size of the induration, measured in millimeters, is crucial for interpreting the test results. Different sizes indicate varying levels of risk for TB infection.
-
Any healthcare provider can read the test results.
The results must be read and reported by a qualified healthcare provider, such as an RN or MD, to ensure accurate interpretation.
-
The expiration date of the test material is irrelevant.
The expiration date is important. Using expired materials can lead to inaccurate results, making it essential to check this date before administration.
-
Positive results always indicate active TB disease.
A positive result suggests a reaction to the test, which may indicate either active TB disease or latent TB infection. Further evaluation is necessary to determine the next steps.
-
Once tested, individuals do not need to be retested.
Depending on risk factors and potential exposure, individuals may need to be retested periodically, especially if they work in healthcare or other high-risk environments.
-
The TB Test form is the same for all types of TB testing.
This form specifically pertains to the Mantoux (PPD) test. Other types of TB tests, such as blood tests, may require different documentation.
Key takeaways
When filling out and using the TB Test form, it’s essential to pay attention to specific details to ensure accuracy and compliance. Here are some key takeaways:
- Complete All Sections: Every part of the form must be filled out. Incomplete forms may not be accepted.
- Identify the Healthcare Professional: Clearly indicate the name and title of the healthcare professional administering the test.
- Specify the Testing Location: Make sure to note where the test is being conducted. This helps in tracking and record-keeping.
- Document the Date Placed: Record the exact date the test is administered. This is crucial for determining the reading time.
- Indicate the Site: Specify whether the test was placed on the right or left arm. This detail is important for accurate follow-up.
- Read the Test Within 48-72 Hours: Ensure the test is read within the specified timeframe to obtain valid results.
- Measure Induration: Accurately measure the induration in millimeters and record this information on the form.
- Report Results Clearly: Indicate whether the PPD (Mantoux) test result is negative or positive, and ensure the signature of the professional reading the results is included.
By following these guidelines, individuals can help ensure that the TB Test form is filled out correctly and used effectively.
File Information
| Fact Name | Description |
|---|---|
| Form Title | This form is officially titled "Tuberculosis Skin Test Form." |
| Healthcare Professional Details | The form requires the name of the healthcare professional administering the test. |
| Testing Location | The location where the test is administered must be recorded. |
| Date Placed | The date when the test is placed must be specified. |
| Site of Injection | The form allows the selection of the injection site, either right or left arm. |
| Lot Number | A lot number for the PPD solution is required for tracking purposes. |
| Expiration Date | The expiration date of the PPD solution must be noted on the form. |
| Date Read | The results must be read and recorded within 48 to 72 hours after placement. |
| Induration Measurement | The induration must be measured in millimeters and recorded accurately. |
| Test Result | The form requires a clear indication of whether the test result is negative or positive. |
| Signature Requirement | Both the administering professional and the person reading the results must sign the form. |