Fill Your Medication Administration Record Sheet Form
Different PDF Templates
Navpers 1336 3 - The form also outlines the expectations regarding professionalism in requests.
Geico Supplement Request - This form must be filled out completely to ensure timely processing of supplement requests.
When engaging in a motorcycle sale, it's important to have a clear understanding of the necessary documentation involved, particularly the Arizona Motorcycle Bill of Sale. This legal form facilitates the transfer of ownership and details key information about the buyer, seller, motorcycle specifics, and sale price. For those looking to ensure a seamless transaction, it can be helpful to reference resources such as the arizonapdfs.com/motorcycle-bill-of-sale-template to obtain the correct documentation and guidelines.
Stock Transfer Form - This ledger should be considered a living document, continuously updated with every transaction.
Similar forms
The Medication Administration Record (MAR) is akin to the Patient Care Record (PCR), which serves as a comprehensive documentation tool for healthcare providers. Both documents track patient care activities, including medication administration, vital signs, and other treatments. While the MAR focuses specifically on medications, the PCR encompasses a broader range of patient interactions, providing a holistic view of the patient's condition and the care provided over time.
Another similar document is the Medication Reconciliation Form, which ensures that a patient’s medication list is accurate and complete at every transition of care. Like the MAR, this form plays a crucial role in preventing medication errors. It requires healthcare providers to compare the patient’s current medications with those prescribed during a new treatment phase, emphasizing the importance of accurate medication administration and continuity of care.
To further assist with the documentation process, healthcare providers can utilize tools such as the Fill PDF Forms, which streamline the creation and management of essential forms like the Medication Administration Record, ensuring accuracy and compliance throughout patient care.
The Treatment Administration Record (TAR) also bears resemblance to the MAR, as it documents various treatments administered to patients, including medications. While the MAR is specifically for medications, the TAR may include other therapeutic interventions, such as physical therapy or wound care. Both documents require meticulous recording of the time and nature of each treatment to ensure compliance with care protocols.
In addition, the Nursing Care Plan (NCP) shares similarities with the MAR in that both outline specific interventions for patient care. The NCP details the nursing strategies and goals for a patient, while the MAR tracks the execution of those strategies, particularly in medication administration. Both documents are essential for ensuring that patient care is systematic and based on established protocols.
The Incident Report Form is another document that aligns with the MAR, albeit in a different context. While the MAR records routine medication administration, the Incident Report Form documents any adverse events or errors related to medication. Both forms contribute to quality assurance in healthcare by identifying areas for improvement and ensuring that proper protocols are followed to enhance patient safety.
Lastly, the Consent for Treatment Form is similar to the MAR in that both require the patient's or guardian's acknowledgment of the care being provided. The Consent Form ensures that patients are informed about the medications they will receive, while the MAR records the actual administration of those medications. Together, these documents uphold the principles of informed consent and patient autonomy in healthcare settings.
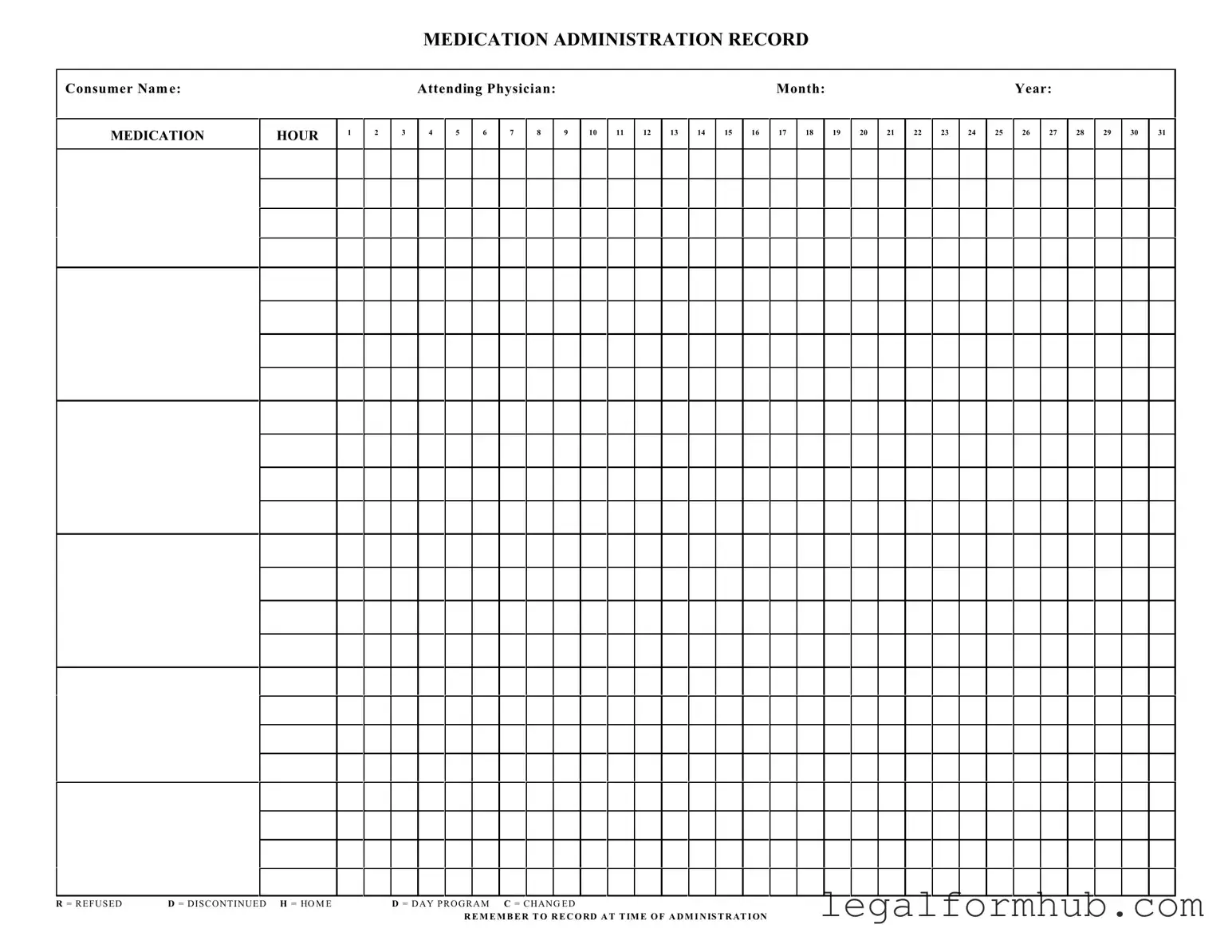
Instructions on Writing Medication Administration Record Sheet
Completing the Medication Administration Record Sheet is essential for tracking medication administration accurately. This process ensures that all necessary information is recorded clearly and systematically, allowing for effective communication among healthcare providers.
- Begin by entering the Consumer Name at the top of the form.
- Fill in the Attending Physician name next to the consumer's name.
- Specify the Month and Year for which the medication record is being filled out.
- In the designated columns, record the medication administration times for each day of the month.
- For each medication hour, mark the appropriate status using the provided codes: R for Refused, D for Discontinued, H for Home, M for Day Program, and C for Changed.
- Ensure to record the information at the time of administration to maintain accuracy.
Misconceptions
Understanding the Medication Administration Record Sheet (MARS) is crucial for anyone involved in patient care. However, several misconceptions often arise. Here are five common misunderstandings:
- It’s only for nurses. Many believe that only nurses can fill out the MARS. In reality, anyone involved in medication administration, including caregivers and aides, can and should use this form to ensure accurate records.
- It’s optional. Some think that using the MARS is optional. This is not true. Accurate documentation is essential for patient safety and compliance with regulations.
- All medications are listed. Many assume that the MARS includes every medication a patient might take. However, it typically only lists medications prescribed for that specific treatment plan. Always verify with the healthcare provider for a complete list.
- Recording is only necessary after administration. Some people believe that recording should happen only after a medication is given. In fact, it’s important to document at the time of administration to ensure accuracy and accountability.
- Refusals and changes don’t need to be noted. A common misconception is that refusing medication or changes in prescriptions don’t require documentation. This is incorrect. Every refusal or change must be recorded to maintain a clear and accurate medical history.
Being aware of these misconceptions can help ensure that the MARS is used effectively and responsibly, ultimately improving patient care.
Key takeaways
Filling out and utilizing the Medication Administration Record Sheet is essential for ensuring proper medication management. Here are some key takeaways to keep in mind:
- Consumer Information: Always start by clearly entering the consumer's name at the top of the form. This ensures that the record is associated with the correct individual.
- Physician Details: Include the name of the attending physician. This provides a point of reference for any medical inquiries or concerns.
- Accurate Dates: Make sure to fill in the month and year accurately. This helps in tracking medication over time and ensures compliance with treatment schedules.
- Hourly Tracking: The form allows for tracking medication at specific hours throughout the day. Be diligent in marking the times when medications are administered.
- Medication Codes: Familiarize yourself with the codes such as R (Refused), D (Discontinued), H (Home), D (Day Program), and C (Changed). Using these codes correctly is crucial for accurate record-keeping.
- Documentation Timing: It is important to record the administration of medication at the time it occurs. This practice enhances accountability and accuracy.
- Consistency is Key: Regularly update the record. Consistency in documentation helps in monitoring the effectiveness of the medication and any side effects.
- Reviewing Records: Periodically review the completed Medication Administration Record Sheets to identify any patterns or issues that may arise.
- Communication: Use the record as a communication tool among caregivers, physicians, and family members. Sharing this information can improve overall care and medication management.
File Information
| Fact Name | Details |
|---|---|
| Purpose | The Medication Administration Record Sheet is used to document the administration of medications to consumers in a healthcare setting. |
| Consumer Identification | The form requires the consumer's name to ensure accurate record-keeping and medication administration. |
| Physician Information | It includes a section for the attending physician's name, which helps in tracking the prescribing authority. |
| Monthly Tracking | The form is designed to track medication administration on a monthly basis, with spaces for each day of the month. |
| Administration Hours | There are designated hours for medication administration, allowing healthcare providers to record the specific time each medication is given. |
| Refusal and Discontinuation Codes | The form includes codes such as R for refused, D for discontinued, and H for home, which are crucial for understanding medication compliance. |
| Change Documentation | Healthcare providers can document any changes in medication or dosage, ensuring that all alterations are recorded accurately. |
| Legal Compliance | In many states, the use of a Medication Administration Record Sheet is governed by healthcare regulations, ensuring adherence to legal standards. |
| Importance of Timely Recording | The form emphasizes the need to record administration at the time it occurs, which is vital for maintaining accurate medical records. |