Fill Your Annual Physical Examination Form
Different PDF Templates
Cadet Command Regulations - The form supports students in organizing their academic schedules effectively.
How to Check How Many College Credits You Have - Complete the Everest University Transcript Request Form for official transcripts.
In addition to the essential protections offered by the California Release of Liability form, individuals can access further resources and templates to facilitate the process. For more information and to find suitable forms, visit pdftemplates.info/, where you can explore various options that can assist in ensuring all participants are aware of their rights and responsibilities during activities.
Uscis Affidavit of Support - The form requests information on assets, such as savings and property.
Similar forms
The Annual Physical Examination form shares similarities with the Medical History Questionnaire. Both documents require patients to provide comprehensive information about their medical history, including past illnesses, surgeries, and current medications. This information is essential for healthcare providers to understand the patient's background and tailor their medical care accordingly. Each form emphasizes the importance of accuracy to avoid misdiagnosis or inappropriate treatments.
Another document akin to the Annual Physical Examination form is the Immunization Record. This record tracks vaccinations a patient has received over time, including dates and types of immunizations. Similar to the physical examination form, it ensures that healthcare providers have an up-to-date understanding of a patient's immunization status, which is crucial for preventing communicable diseases and managing public health.
The Consent for Treatment form also bears resemblance to the Annual Physical Examination form. Both documents require the patient’s personal information and consent to proceed with medical evaluations or treatments. This consent is vital for legal and ethical reasons, ensuring that patients are informed about the procedures they will undergo and the potential risks involved.
The Health Risk Assessment form is another document that aligns closely with the Annual Physical Examination form. It evaluates a patient's lifestyle choices, family history, and other factors that may impact their health. Both forms aim to identify potential health risks early, allowing for proactive management and intervention.
Similar to the Annual Physical Examination form is the Laboratory Test Requisition form. This document is used to request specific laboratory tests based on the findings of a physical examination. Both forms are integral to the diagnostic process, ensuring that the healthcare provider has the necessary information to make informed decisions about patient care.
The Referral Form for Specialist Consultation is another comparable document. When a primary care physician identifies a need for specialized care, they complete this form, which includes patient information and the reason for the referral. Like the Annual Physical Examination form, it facilitates communication between healthcare providers to ensure coordinated care for the patient.
The Patient Information Form also shares characteristics with the Annual Physical Examination form. Both require detailed personal and medical information from the patient. This information helps healthcare providers understand the patient's unique health profile, which is essential for delivering personalized care and addressing specific health concerns.
The Emergency Contact Form is yet another document that resembles the Annual Physical Examination form. While the latter focuses on health assessments, both documents require the collection of personal information, including emergency contacts. This information is critical for healthcare providers in case of urgent medical situations, ensuring that the patient's wishes and preferences are respected.
To establish your corporation efficiently, be sure to review our guidance on essential Articles of Incorporation requirements found at essential Articles of Incorporation guidelines.
The Medication Reconciliation Form is similar in that it documents a patient’s current medications and any changes made during their visit. Both forms emphasize the importance of accurate medication lists to avoid adverse drug interactions and ensure safe prescribing practices.
Lastly, the Discharge Summary is akin to the Annual Physical Examination form in that it summarizes a patient's health status and recommendations for follow-up care. Both documents serve as critical tools for communication between healthcare providers and patients, ensuring that all parties are informed about the patient's health and necessary next steps.
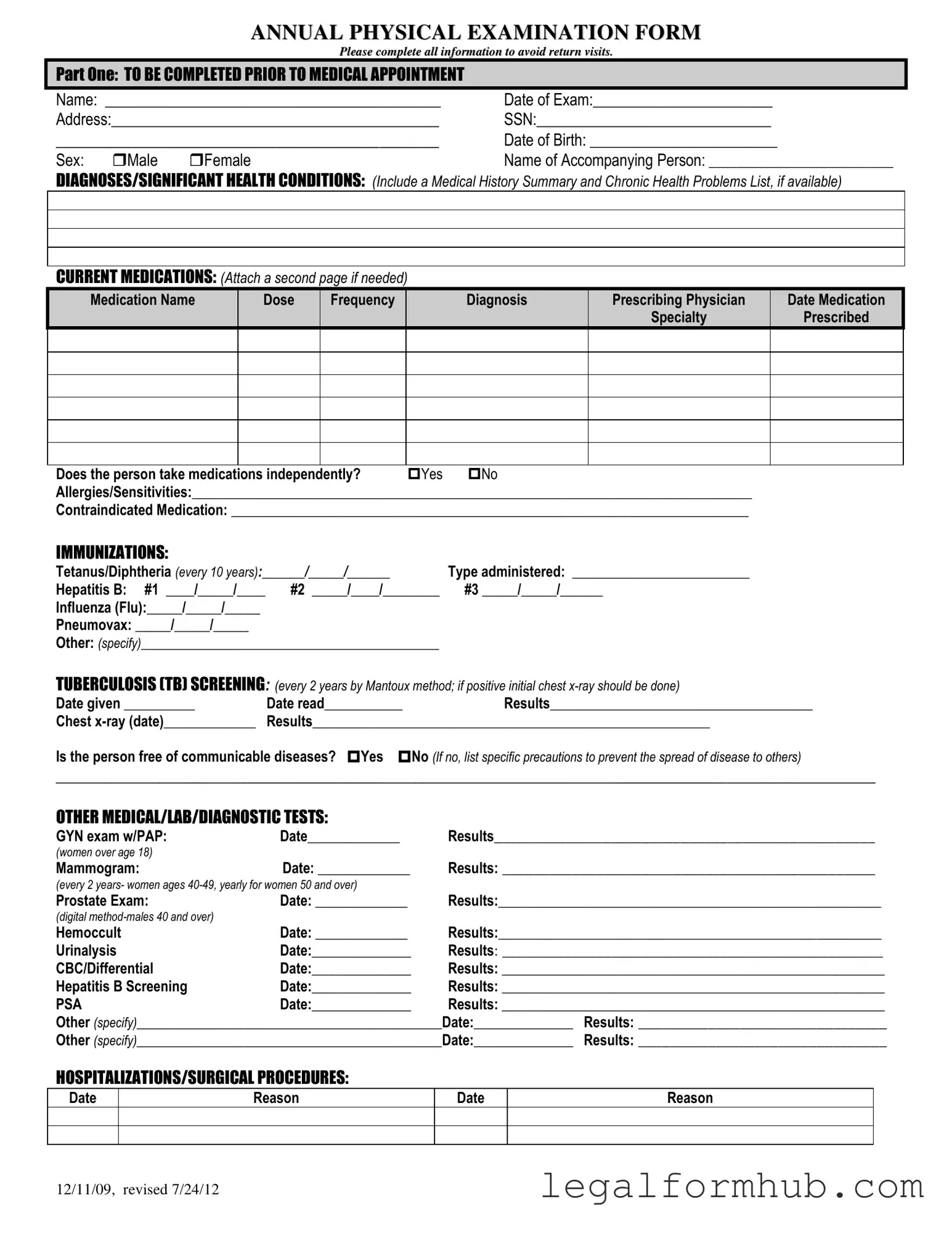
Instructions on Writing Annual Physical Examination
Completing the Annual Physical Examination form is an important step in ensuring your health needs are accurately documented. After filling out the form, you’ll be ready to present it to your healthcare provider during your appointment. This will help streamline your visit and ensure that all necessary information is available for your examination.
- Personal Information: Fill in your name, date of exam, address, Social Security Number (SSN), date of birth, and sex (check the appropriate box).
- Accompanying Person: If someone is accompanying you, write their name in the provided space.
- Health Conditions: List any significant health conditions or diagnoses. Include a summary of your medical history and any chronic health problems if you have that information available.
- Current Medications: List all medications you are currently taking. Include the medication name, dose, frequency, diagnosis, prescribing physician, and date prescribed. If necessary, attach a second page.
- Medication Independence: Indicate whether you take medications independently by checking "Yes" or "No."
- Allergies: Write down any allergies or sensitivities you have.
- Contraindicated Medication: List any medications that are contraindicated for you.
- Immunizations: Fill in the dates and types of immunizations you have received, such as Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax.
- TB Screening: Record the date the TB test was given and read, along with the results. If a chest x-ray was done, include the date and results as well.
- Communicable Diseases: Indicate whether you are free of communicable diseases and list any precautions if applicable.
- Medical Tests: Document any additional medical, lab, or diagnostic tests you have undergone, including dates and results.
- Hospitalizations/Surgical Procedures: Note any hospitalizations or surgeries, including the date and reason for each.
- General Physical Examination: Complete the section on blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluation of Systems: For each system listed, indicate whether the findings were normal by checking "Yes" or "No" and provide comments as needed.
- Vision and Hearing Screening: Indicate whether screenings were performed and if further evaluation is recommended.
- Additional Comments: Provide any relevant comments, including medical history review, medication changes, health maintenance recommendations, and any limitations or restrictions for activities.
- Adaptive Equipment: Indicate if you use any adaptive equipment and specify what it is.
- Change in Health Status: Note any changes in your health status from the previous year.
- Physician Information: Print the name of your physician, sign the form, and include the date, physician address, and phone number.
Misconceptions
Misconceptions about the Annual Physical Examination form can lead to confusion and incomplete submissions. Below are nine common misconceptions along with clarifications.
- All sections must be filled out for every appointment. While it is important to provide as much information as possible, not every section applies to every individual. Focus on relevant health conditions and medications.
- The form is only necessary for new patients. This is incorrect. Existing patients should also complete the form annually to ensure all health information is up-to-date.
- Medications do not need to be listed if they have not changed. In fact, it is advisable to list all current medications, regardless of changes, to provide a complete picture of the patient's health.
- Immunization history is optional. Immunization records are crucial for assessing overall health and determining necessary vaccinations. This section should be completed thoroughly.
- Only primary care physicians review this form. Specialists may also review the information provided to tailor their care to the patient's specific needs.
- All tests listed are mandatory. The tests mentioned in the form are recommended based on age and health history. However, not all patients will require every test.
- Submitting the form guarantees a thorough examination. The form is a tool to assist healthcare providers. A thorough examination still depends on the provider's assessment during the appointment.
- All information is kept confidential. While patient privacy is a priority, certain information may be shared with healthcare professionals involved in the patient's care as needed.
- There is no need to update the form if health status changes. Changes in health status should be documented immediately to ensure accurate care and recommendations are provided.
Understanding these misconceptions can enhance the effectiveness of the Annual Physical Examination process and contribute to better health outcomes.
Key takeaways
Filling out the Annual Physical Examination form accurately is crucial for a smooth medical appointment. Here are some key takeaways to keep in mind:
- Complete All Sections: Ensure that every section of the form is filled out completely. Missing information may lead to delays or the need for additional visits.
- Provide a Detailed Medical History: Include any significant health conditions, past surgeries, and current medications. This helps your healthcare provider understand your health better.
- List Allergies and Sensitivities: Clearly note any allergies or sensitivities to medications. This information is vital for your safety during treatment.
- Stay Updated on Immunizations: Record your immunization history accurately. Knowing your vaccination status can influence the care you receive during your visit.
By following these guidelines, you can help ensure that your physical examination goes smoothly and that your healthcare provider has all the information needed to provide the best care possible.
File Information
| Fact Name | Description |
|---|---|
| Purpose of the Form | The Annual Physical Examination Form is designed to gather comprehensive health information to ensure accurate assessments during medical appointments. |
| Personal Information Required | Patients must provide essential personal details, including name, date of birth, address, and social security number, to facilitate proper identification and record-keeping. |
| Medication Disclosure | Patients are asked to list current medications, including dosage and prescribing physician, to ensure safe and effective treatment plans. |
| Immunization Records | The form includes sections for documenting immunizations, such as Tetanus and Hepatitis B, which are crucial for maintaining public health standards. |
| Screening Tests | Various screenings, including TB tests and GYN exams, are recommended based on age and gender, helping to identify health issues early. |
| Health Maintenance Recommendations | After the examination, physicians provide tailored recommendations for health maintenance, including diet, exercise, and follow-up lab work. |
| Legal Considerations | In many states, specific laws govern the use and storage of medical forms, ensuring patient privacy and the secure handling of health information. |
| Signature Requirement | Finally, the form requires the physician's signature, confirming that the examination and recommendations were conducted and discussed with the patient. |